58% of US consumers now prioritize personal health and wellness more than last year, yet many still report unsatisfying healthcare experiences. That gap places constant pressure on you to deliver better care while meeting operational demands with limited time, staff, and clarity.
You face competing priorities across clinical teams and operations, unclear ownership, and goals that drift apart despite strong intentions. When outcomes disappoint, accountability blurs, and momentum stalls, leaders often feel stuck choosing between patient care and operational progress.
In this blog, we’ll explore how OKRs for healthcare organizations support aligning clinical and operational goals through clear examples and practical steps. You’ll see how this approach sharpens focus, assigns ownership, and supports better decisions without adding extra process layers.
Key Takeaways:
- OKRs help you connect clinical priorities and operational goals through shared outcomes that leaders and teams can review consistently.
- KPIs track ongoing performance, while OKRs set direction and guide decisions when tradeoffs arise across care delivery and operations.
- Effective healthcare OKRs focus on outcomes, limit objectives, and assign clear ownership to prevent confusion and stalled progress.
- Most OKR failures in healthcare come from unclear ownership, too many priorities, and treating objectives like static metrics.
- Leadership commitment and visible review rhythms determine whether OKRs become a decision system or fade into routine reporting.
What OKRs Mean for Healthcare Organizations
OKRs give healthcare organizations a clear structure for setting priorities, defining success, and tracking progress across clinical and operational teams. They shift focus away from scattered activities and toward outcomes that leaders, managers, and care teams can clearly understand and act on.
For you, OKRs create shared clarity across departments by linking patient care goals with operational expectations. They help leaders set direction, managers guide execution, and teams see how their daily work supports broader organizational goals.
Now that you understand how OKRs function in healthcare, reviewing practical examples helps you see how leaders apply them across departments.
Also Read: Why Are OKRs Important for Business Success? 12 Practical Reasons That Prove It
10 High-Impact OKR Examples for Healthcare Organizations
Below are ten practical OKR examples designed for healthcare organizations, balancing patient care expectations with operational responsibilities across leadership and departmental teams.
1. Objective: Improve patient experience across all care settings during the quarter.
- Key Result 1: Increase patient satisfaction survey scores from discharge follow-ups by ten percent across inpatient and outpatient services.
- Key Result 2: Reduce average complaint resolution time from seven days to three days through clearer ownership and escalation paths.
2. Objective: Reduce avoidable hospital readmissions within thirty days of discharge.
- Key Result 1: Decrease thirty-day readmission rates for high-risk conditions by fifteen percent through improved discharge planning.
- Key Result 2: Ensure ninety percent of discharged patients receive follow-up contact within forty-eight hours after leaving care.
3. Objective: Strengthen care team accountability for clinical quality outcomes.
- Key Result 1: Assign single accountable owners for each clinical quality objective across departments before the quarter begins.
- Key Result 2: Review clinical outcome data with department heads during scheduled monthly performance check-ins.
4. Objective: Improve access to care for new and existing patients.
- Key Result 1: Reduce average appointment wait times for priority services by twenty percent across all locations.
- Key Result 2: Increase same-week appointment availability by adding structured scheduling blocks for urgent patient needs.
5. Objective: Improve staff engagement and retention among clinical teams.
- Key Result 1: Increase quarterly engagement survey participation rates to at least eighty-five percent across all care teams.
- Key Result 2: Reduce voluntary clinician turnover by ten percent through clearer workload expectations and feedback cycles.
6. Objective: Improve coordination between clinical and administrative teams.
- Key Result 1: Conduct monthly joint planning sessions between clinical leaders and operations managers for shared priorities.
- Key Result 2: Document and communicate agreed priorities within five business days following each planning session.
7. Objective: Improve documentation accuracy and timeliness across care teams.
- Key Result 1: Reduce incomplete clinical documentation incidents by twenty percent through regular audits and targeted coaching.
- Key Result 2: Ensure ninety-five percent of clinical notes are completed within twenty-four hours of patient encounters.
8. Objective: Strengthen leadership visibility into organizational priorities and progress.
- Key Result 1: Establish a single quarterly review cadence where leadership reviews progress against stated objectives.
- Key Result 2: Ensure all department heads report progress using the same format during leadership review meetings.
9. Objective: Improve financial predictability without compromising care quality.
- Key Result 1: Reduce cost overruns in priority service lines by twelve percent through better planning and monitoring.
- Key Result 2: Improve forecast accuracy for staffing costs within five percent variance each quarter.
10. Objective: Build consistent goal-setting habits across departments.
- Key Result 1: Train one hundred percent of department heads on writing outcome-focused objectives before the next cycle.
- Key Result 2: Ensure every department publishes no more than three objectives for the quarter with clear ownership defined.
After reviewing these examples, you may wonder when OKRs work better than traditional performance indicators in healthcare environments.
Also Read: Fuel Your OKR Engine: From Inputs to Impact – A Journey Powered by Activities, Outputs, and Outcomes
When to Use OKRs vs KPIs in Healthcare Settings
KPIs and OKRs serve different purposes in healthcare, and confusion between them often leads to unclear priorities and stalled progress. KPIs track ongoing performance, while OKRs define directional goals that guide clinical and operational decisions across leadership levels.
To clarify how each works and when to use them, here are the key differences side by side.
| Aspect | OKRs | KPIs |
| Primary purpose | Set direction and define desired outcomes | Measure ongoing performance |
| Time horizon | Fixed cycle, usually quarterly | Continuous and long-term |
| Focus | Change and progress toward specific goals | Stability and monitoring |
| Scope | Cross-functional and organization-wide | Departmental or role-specific |
| Ownership | Single accountable owner per objective | Often shared across teams |
| Use in healthcare | Drive improvements in care delivery and operations | Track metrics like wait times or readmission rates |
| Relationship to goals | Describe what you want to achieve and how success looks | Show whether current processes meet targets |
Understanding this difference matters most when you bring clinical and operational leaders together around shared priorities.
Also Read: How to Implement Key Performance Indicators (KPIs) Effectively
How OKRs Align Clinical and Operational Goals
Clinical teams and operational leaders often work toward related outcomes but measure success in different ways, which creates tension and slows progress. OKRs connect both sides through shared objectives, helping you balance patient care expectations with operational commitments without forcing tradeoffs.
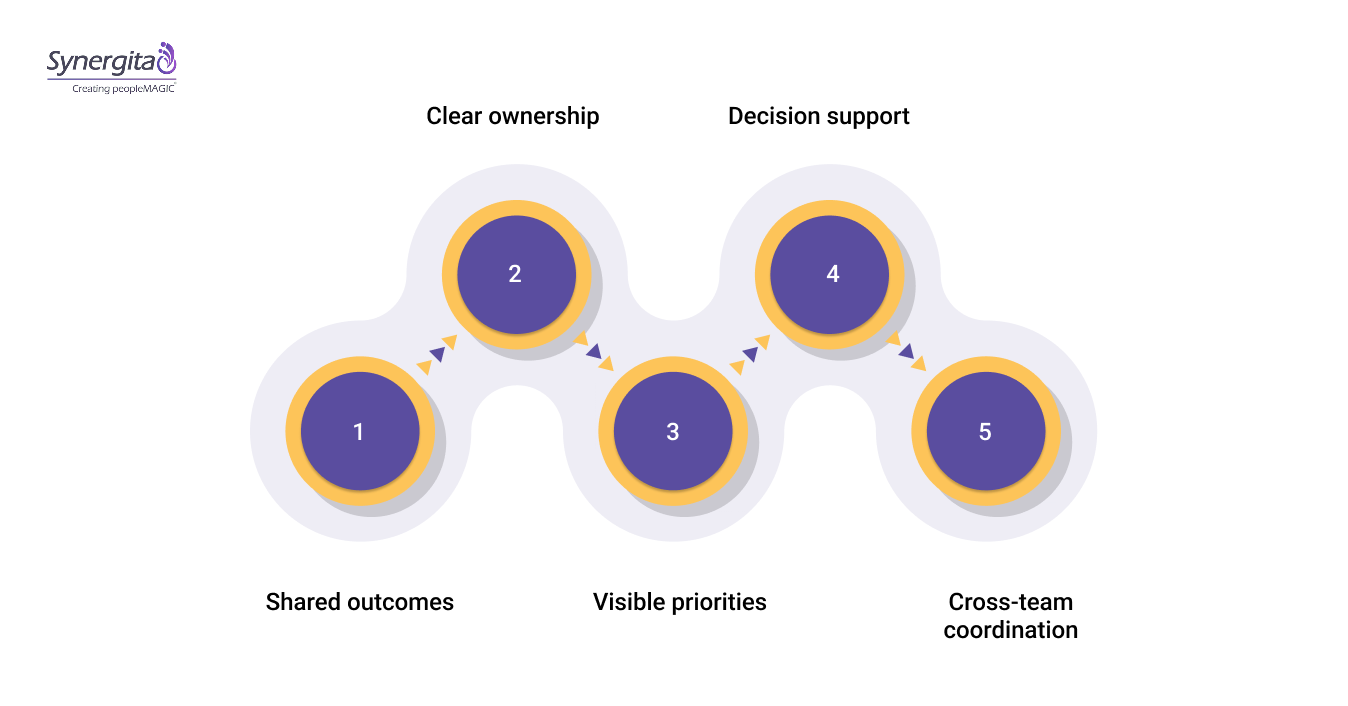
To make this connection clear and actionable, here are the core ways OKRs bring both groups onto the same page:
- Shared outcomes: Clinical quality goals and operational targets roll up into one objective that reflects what success looks like for the entire organization.
- Clear ownership: Each objective has one accountable owner, reducing confusion between clinical leadership and operational management.
- Visible priorities: Teams see which goals matter most each cycle, limiting distractions from low-impact initiatives.
- Decision support: When resources feel constrained, OKRs guide choices by showing which actions directly support stated objectives.
- Cross-team coordination: Departments plan work around common objectives, reducing conflicts between care delivery and administrative demands.
Understanding this relationship prepares you to create OKRs that reflect both clinical and operational priorities.
Also Read: 10 Key Benefits of OKRs Software for Business Growth
A Step-by-Step Guide to Writing Healthcare OKRs
Writing effective healthcare OKRs requires discipline, clarity, and restraint, especially when clinical outcomes and operational expectations compete for attention. A step-by-step approach helps you define goals that teams understand, and that leaders can review with confidence.
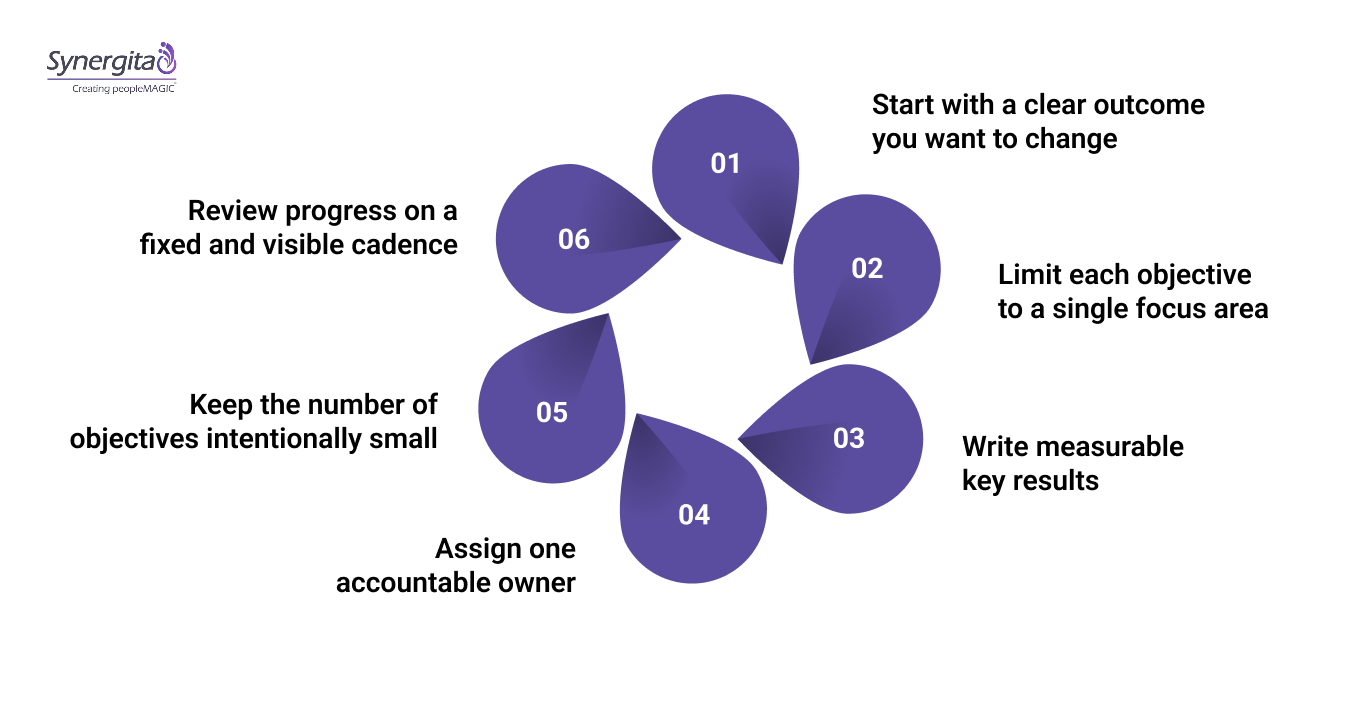
1. Step 1: Start with a clear outcome you want to change.
Define an objective that describes a meaningful outcome for patients, staff, or operations, rather than listing tasks or activities your teams already perform.
2. Step 2: Limit each objective to a single focus area.
When objectives try to cover too much, teams lose clarity, and progress becomes difficult to assess during regular reviews.
3. Step 3: Write measurable key results tied to observable change.
Each key result should describe a specific shift in results, using numbers, percentages, or timeframes that teams can track consistently.
4. Step 4: Assign one accountable owner for every objective.
Clear ownership prevents confusion between clinical leaders and operational managers when priorities conflict or decisions require escalation.
5. Step 5: Keep the number of objectives intentionally small.
Most healthcare teams perform best with one to three objectives per cycle, which protects focus and reduces competing priorities.
6. Step 6: Review progress on a fixed and visible cadence.
Regular check-ins help leaders address risks early while reinforcing shared responsibility for outcomes across departments.
Even well-written OKRs can fail when teams repeat common mistakes during setup, ownership, or review cycles.
Also Read: OKR Best Practices 2026: Tips to Set and Achieve Better Goals
Common OKR Mistakes Healthcare Leaders Should Avoid
Many healthcare organizations struggle with OKRs not because the framework fails, but because common mistakes weaken focus and accountability from the start. These issues often create confusion between clinical teams and operations, leading to frustration during reviews.
To avoid these setbacks, here are the most frequent OKR mistakes seen in healthcare settings:
- Treating OKRs like KPIs: Teams turn objectives into status metrics, which removes direction and limits meaningful progress.
- Setting too many objectives: When priorities multiply, teams lose focus and struggle to make tradeoffs during daily work.
- Unclear ownership: Shared responsibility without a single owner leads to delays and unresolved decisions.
- Activity-based key results: Listing tasks instead of outcomes makes progress hard to evaluate during check-ins.
- Skipping regular reviews: Without consistent check-ins, risks surface late and objectives lose relevance over time.
Avoiding these mistakes starts with leadership setting expectations and modeling disciplined goal-setting behavior.
Also Read: Top 10 OKR Mistakes and How to Avoid Them
How Leaders Should Roll Out OKRs
Leaders play a decisive role in whether OKRs gain traction or fade after early enthusiasm across healthcare teams. You set the tone by clearly stating priorities, limiting objectives, and reinforcing that OKRs guide decisions rather than serve as reporting artifacts.
A structured rollout works best when leaders begin with a shared planning session, publish clear objectives, and commit to visible review rhythms. Some teams support this process with tools like Syenergita to maintain consistency, track progress, and keep discussions focused on outcomes during leadership check-ins.
Conclusion
Clear goals matter most when patient care and operational priorities pull teams in different directions. OKRs for healthcare organizations give you a practical way to set direction, clarify ownership, and review progress without adding confusion or noise.
When leaders use OKRs as a shared decision system, aligning clinical and operational goals becomes easier, helping teams stay focused, improve reviews, and manage tradeoffs across daily work.
Start your free trial with Syenergita and turn disconnected goals into shared clarity across your healthcare organization.
FAQs
1. What are clinical OKRs?
Clinical OKRs define outcome-focused goals tied directly to patient care, safety, or clinical quality, with measurable results that show progress without relying on task lists. They help clinical leaders track improvement areas while keeping care standards clear and reviewable across teams.
2. What is OKR alignment?
OKR alignment refers to connecting goals across leadership, departments, and teams so everyone works toward the same outcomes during a defined cycle. It ensures individual and team objectives support higher-level priorities rather than competing with them.
3. What are SMART goals for healthcare organizations?
SMART goals describe targets that are specific, measurable, achievable, relevant, and time-bound, often used for operational planning or compliance tracking. They work well for defined tasks, while OKRs focus more on directional outcomes and progress.
4. What are some good OKR examples?
Good OKRs clearly state the outcome to change and include key results that show measurable improvement within a set timeframe. They avoid task lists and focus on results leaders can review, and teams can influence directly.
5. What are the 5 P’s of goal-setting?
The five Ps commonly refer to purpose, priorities, people, process, and progress, which guide how goals are set and reviewed. This framework helps leaders think through why a goal matters, who owns it, and how success gets measured.

